Monday, December 31, 2007
Tips for identifying the symptoms of alcoholism
What is alcoholism?
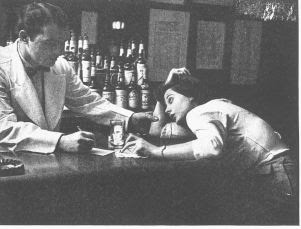
Alcoholism is the inability to control alcohol intake. A person might suffer constant preoccupation with drinking, which can lead to personal, medical, professional and financial problems. Impairment can range from intermittent loss of control to substantial physical and mental impairment or death.
About 18 million people suffer from alcoholism, and about 100,000 people die from alcohol-related medical problems each year in the United States. Half of all traffic deaths are related to alcohol.
Not a shift passes in the emergency department without me treating a patient for alcohol-related complaints. The most difficult situations for me to deal with are alcohol-related traffic fatalities.
What are the symptoms?
Routinely drinking alone, consuming alcohol at all times of the day, becoming angry when drinking habits are questioned and persistent drinking leading to loss of memory or blackouts can be signs of a problem. As alcoholism progresses, a person can lose interest in family, friends and hobbies; eventual problems with employment might occur. Altered personality, shaking, irritability, sweating and seizures are all signs of withdrawal.
What are the causes?
Research shows alcohol addiction is a physical problem. Genetics play a strong role. Drinking at an early age also places one at risk for becoming an alcoholic, as does gender: Men have a greater risk of alcoholism than women.
What is the treatment?
Identifying the problem can be difficult because patients with alcohol problems tend to deny their intake. In some cases, withdrawal only becomes evident when alcohol is unavailable, such as hospitalization.
Outpatient counseling and abstinence might work for people without underlying medical problems. Support groups are quite effective in maintaining sobriety.
Patients with other medical problems might need to be hospitalized. Doctors can treat potentially life-threatening withdrawal with medications; once medically stabilized, a patient may choose to pursue an inpatient detoxification program; the length might vary depending on the problem's severity.
A recent study indicated the anti-seizure medication gabapentin might help with alcohol abstinence. Other medications also work to help severe alcoholics who relapse.
As you celebrate the new year, please drink sensibly. And, as always, never drink and drive because the consequences may be with you for a lifetime.
source: Dr. Randal F. Wojciehoski (also known as Dr. Wojo) is a Stevens Point native and an emergency medicine department physician at Saint Michael's Hospital.
Friday, December 28, 2007
Modified Protein May Lead to First Cure for Cirrhosis
Six years ago, the UC San Diego School of Medicine research team discovered the cause of the excess fibrous tissue growth that leads to liver fibrosis and cirrhosis, and developed a way to block excess scar tissue in mice. At that time, the best hope seemed to be future development of a therapy that would prevent or stop damage in patients suffering from the excessive scarring related to liver or lung disease or severe burns.
In their current study, Martina Buck, Ph.D., assistant professor of medicine at UCSD and the Veterans Affairs San Diego Healthcare System, and Mario Chojkier, M.D., UCSD professor of medicine and liver specialist at the VA, show that by blocking a protein linked to overproduction of scar tissue, they can not only stop the progression of fibrosis in mice, but reverse some of the cell damage that already occurred.
In response to liver injury -- for example, cirrhosis caused by alcohol -- hepatic stellate cell (HSC) activated by oxidative stress results in large amounts of collagen. Collagen is necessary to heal wounds, but excessive collagen causes scars in tissues. In this paper, the researchers showed that activation of a protein called RSK results in HSC activation and is critical for the progression of liver fibrosis. They theorized that the RSK pathway would be a potential therapeutic target, and developed an RSK inhibitory peptide to block activation of RSK.
The scientists used mice with severe liver fibrosis -- similar to the condition in humans with cirrhosis of the liver -- that was induced by chronic treatment with a liver toxin known to cause liver damage. The animals, which continued on the liver toxin, were given the RSK-inhibitory peptide. The peptide inhibited RSK activation, which stopped the HSC from proliferating. The peptide also directly activated the caspase or "executioner" protein, which killed the cells producing liver cirrhosis but not the normal cells.
"All control mice had severe liver fibrosis, while all mice that received the RSK-inhibitory peptide had minimal or no liver fibrosis," said Buck.
Buck explained that the excessive collagen response is blocked by the RSK-inhibitory peptide, but isn't harmful to the liver. "The cells continue to do their normal, healing work but their excess proliferation is controlled," Buck said. "Remarkably, the death of HSC may also allow recovery from liver injury and reversal of liver fibrosis."
The researchers found a similar activation of RSK in activated HSC in humans with severe liver fibrosis but not in control livers, suggesting that this pathway is also relevant in human liver fibrosis. Liver biopsies from patients with liver fibrosis also showed activated RSK.
The study expands on work reported in 2001 in the journal Molecular Cell announcing that a team led by Buck had found that a small piece of an important regulatory protein called C/EBP beta was responsible for fibrous tissue growth, or excessive scar tissue following injury or illness. When normal scarring goes awry, excessive build-up of fibrous tissue can produce disfiguring scars or clog vital internal organs and lead to serious complications. Buck and colleagues developed a mutated protein that stopped this excessive fibrous tissue growth.
"Six years ago, we showed a way to prevent or stop the excessive scarring in animal models," said Buck. "Our latest finding proves that we can actually reverse the damage."
Worldwide, almost 800,000 people die from liver cirrhosis each year, and there is currently no treatment for it. Excessive tissue repair in chronic liver disease induced by viral, toxic, immunologic and metabolic disorders all result in excessive scar tissue, and could benefit from therapy developed from the UCSD researchers' findings.
The research was supported by grants from the National Institutes of Health, the Department of Veterans Affairs and UCSD's Medical Research Foundation. Buck is the recipient of a Howard Temin Award from the National Cancer Institute.
Adapted from materials provided by University of California - San Diego.
Wednesday, December 26, 2007
We are all paying the price for cheap alcohol
ALCOHOL Focus Scotland believes urgent government action is required to address the ridiculously low price of alcohol.
Once again, in the run-up to Christmas and New Year, supermarkets are promoting a "booze bonanza" where beer is cheaper than water.
Tesco is offering 60 440ml cans of lager for £20 – just 33p per can – and the most prominent image on the home page of the Asda website is a special offer of three bottles of wine for £10 and two bottles of spirits for £18.
Such promotions are blatantly designed to sell more alcohol.
Alcohol is not an ordinary commodity like tins of soup or loaves of bread. It is a drug which causes increasing harm in our communities. Is it ethical to promote a product so cheaply which has the potential to wreck lives?
The vast majority of alcohol sold for drinking at home is through just six supermarket chains. Supermarkets
need to stop hiding behind arguments that they are responsible merely because they are committed to preventing under-age sales and have signed up to voluntary codes of practice.
The effect of price on alcohol consumption is one of the most researched areas of alcohol policy. The evidence from many international studies is that an overall price increase leads to a reduction in sales, in turn, leading to a reduction in alcohol-related harm. Alcohol overall is now 62 per cent more affordable than in 1980. We are most concerned about drinks that are designed to be drunk quickly or that are particularly strong, such as white ciders.
We are not calling for blanket tax increases but rather additional tariffs on some types of products and an end to the common supermarket practice of below cost sales. Ireland has successful experience of both.
When it removed the tax advantage on cider compared with beer, there was an almost immediate downturn in cider sales. A similar approach could be taken in the UK.
Some say there'
s no reason why responsible drinkers should be prevented from getting a "bargain". But harmful alcohol use is rarely an individual problem – the drinker's behaviour impacts on their children, partner, friends, colleagues and society as a whole.
Others argue that alcohol is cheaper in countries such as Spain or Italy, yet they don't experience the same problems of drunkenness as us. This must be considered in the context of our very different drinking cultures.
The low cost and widespread availability of alcohol in the UK is set against a long-standing culture of social acceptability of drunkenness.
We support Justice Secretary Kenny MacAskill's intention to end cheap price promotions.
At a cost of over £1 billion per year and rising, Scotland can no longer afford to pay such a high price for our drinking culture.
Jack Law is the chief executive of Alcohol Focus Scotland
source: http://news.scotsman.com/
Sunday, December 23, 2007
Remembering the homeless with a vigil

NASHUA – Shivering in 18-degree air on the steps of City Hall on Friday night, Peter Kelleher struggled to light a candle.
"It gives you an idea of how difficult it is to do something in the cold," Kelleher, the president and CEO of Harbor Homes Inc., told the 10 or so other people who were also attempting to light candles in honor of National Homeless Person's Memorial Day.
Information gathered from area agencies that work with the homeless population shows that at any point in time an average of 500-600 homeless people are living in the Greater Nashua area.
"In the 26 years I have been doing this, I have see a lot of people come and go," Kelleher said prior to the start of the half-hour-long vigil.
The vigil, mostly attended by those who work with the local homeless community, featured prayers and a reading of the names of 141 deceased New Hampshire residents known to have struggled with homelessness at some time in their lives.
The vigil began with a moment of silence for the local homeless population and the nine Nashua residents, some homeless or formerly homeless, who died this year.
Among the recently deceased was Ray Larocque, 39, a father of three who died Nov. 11 of a drug overdose. Larocque participated in last year's vigil, breaking into tears when he read the name of Dan Lessard, a homeless friend of his who died in 2005 at the age of 28.
Like many of the chronically homeless, Larocque's periods of homelessness stemmed from his battle with drugs and alcohol.
Following the 2006 vigil, Larocque, who was three months' sober at the time, explained the struggle of trying to land a job without a permanent address, phone number or even clean clothes for an interview.
"People just don't understand," Larocque said.
"It's the way society looks at you."
It's a sentiment that Ken Lewis, program director of Connections, can relate to on a personal level.
Lewis, 47, who works with the homeless through the Harbor Homes' program, estimated he had spent a quarter of his life homeless due to a drug and alcohol problem.
"I was living in an old burned out house," Lewis said, describing his worst day as a homeless person in Nashua in 1994.
"I had nothing to eat, and I just remember being cold and hungry . . . I broke down crying. I didn't want to live like that anymore."
For Lewis, help came with a bed at Keystone Hall, a local substance abuse treatment program where he was able to detoxify his body of drugs and alcohol while living among other addicts who were trying to improve their lives.
"I was lucky," Lewis said.
"Nowadays, you don't have that many beds," he said, describing how homeless addicts in the same situation today often spend weeks waiting to get such help.
Even for those without chemical addictions, shelter is scarce.
Local shelters admit people between the hours of 5:30 and 6:30 p.m., Lewis said, and often end up turning people away, directing them to call city welfare, which closes its doors at 4 p.m.
Lewis said he often directs people to go to city welfare before 3 p.m. to get assistance in getting a spot in the shelter, and if that is not possible, a room for the night, as is required.
There are still people spending nights on the streets, however, and some, despite the recent snow, are spending those nights tented in the woods, he said.
Mark Vallee, 48, a self-described alcoholic who has been homeless since 1985, has lost at least one homeless friend to the elements and even had a close call of his own once.
"I think God was looking out for me that night," Vallee said of a night he spent in a tent in weather that was below zero in the double digits.
"I had one blanket. I got up in the morning, and I couldn't walk. I felt paralyzed," he said.
Vallee was one of three homeless people who showed up to the vigil. Also attending was Dan Kovich, 47, who is going on his third year of chronic homeless in the city.
Kovich, who was planning to spend the night in a nearby shelter, said he was making more than $33 an hour when he lost his job two and half years ago.
Kovich, who has had a prosthetic leg for most of his life and said he suffers from major bi-polar disorder and panic attacks, credits his "street survival skills" for getting him through the hardest days and nights.
"Knowing how to get a free meal, sleeping in laundromats," he explained.
Panhandling is an act of desperation, Kovich said, since people often ignore it.
Like many of the participants of the vigil, Kovich said the city needs more programs to help the homeless and the conditions that often cause homelessness.
The brief vent of frustration prompted Kovich to expel a deep sigh.
"The name of the game is survival," he said. "It's hard being homeless."
source: http://www.nashuatelegraph.com/apps/pbcs.dll/frontpage
By STEPHANIE HOOPER, Telegraph Staff
shooper@nashuatelegraph.com
Saturday, December 22, 2007
SoberCircle Celebrates One Year Connecting the Online Addiction Recovery Community
The site features interactive member profile pages, member-created blogs, special interest groups, forums and chat rooms, among other features. Resources include directories with contact information for thousands of treatment centers and interventionists, an events calendar listing recovery-related events and an online store sells books, CDs and other recovery-related merchandise.
SoberCircle has seen rapid growth since its launch, and has attracted a loyal member following.
"People are so grateful to have a place to come to find others they can easily relate to -- others who are sober or who are seeking sobriety. We have several members who have taken the initiative to organize daily online 12-step meetings," said Chris Ennis, co-founder and lead developer for SoberCircle. "It's so fulfilling to know that our members have a place they can go at any time, day or night, to get support and interact with others who share their same struggles with addiction."
source: http://www.pr-usa.net/
Thursday, December 20, 2007
Staying Sober
body, mind and spirit. It’s important to repair as much as possible of the damage
done by old habits, build new and healthier habits and use the time formerly taken
by drinking or drug-taking for constructive ends.
If you or someone you know is recovering from a chemical habit, here are some
suggestions that can help maintain sobriety.
Taking Good Care of Yourself
First of all, do your best for your body. It probably suffered some setbacks during
your drug-taking days. Get plenty of rest, eat a nutritious diet and exercise regularly.
Rest, food and exercise all affect our moods, as well as our physical well-being.
The best diet is one that’s high in fresh vegetables and whole grains and low in
fats, sugar, additives, red meat and caffeine. Exercise can be of any type that appeals
to the person who’s doing it. It’s safest to increase the amount of exercise gradually
from a gentle beginning, rather than starting out with a strenuous regime.
Learning and Doing
Chances are, your old way of life had many destructive aspects. The more you
understand how old habits of thought and action contribute to dependency, the better
chance you’ve got to change those habits. Perhaps you were always setting yourself
up to fail by making your goals unreasonably high, or you didn’t know how to
have fun or relax, except by getting intoxicated. Maybe you had trouble being honest.
Or your ways of communicating with others were ineffective.
The best way to start the process of change is by trying something new. Learning
and doing are great ways to feel better about yourself and your life. Set yourself a
goal you know you can reach, sign up for a class in something you’ve always wanted
to learn, practice telling yourself the truth about how you feel or try meditation as a
nonchemical way of managing stress. Find out about communication workshops,
see a counselor or attend a meeting of Alcoholics or Narcotics Anonymous. Think
about the person you’d like to be and the life you’d like to lead. Take one small step
today.
Your Highest Priority
Above all, make staying sober your highest priority. Think of the situations that
result in your drinking or taking other drugs, and avoid those situations, as well as
any “old friends” who don’t support you in sobriety. Cultivate a spiritual life in
whatever faith you choose. When faced with a decision, ask yourself which option
will be most helpful in staying sober.
Attend 12-step program meetings regularly. You can get referrals to local groups
from your employee assistance program or the telephone directory. In general, put
your time and your strength into activities and relationships that help you stay
sober. You, and everyone around you, will benefit in the form of happier and
healthier lives.
Wednesday, December 19, 2007
Binge drinking behind sexual health 'epidemic'
Binge drinking among women is causing an epidemic of unwanted pregnancies and sexually transmitted infections, doctors have warned.
Research has found that almost nine in ten women who attended a sexual health clinic admitted binge drinking - an average of two and a half bottles of wine in one sitting.
Doctors blame binge drinking among women for "epidemic" in STIs and unwanted pregnancies
Three quarters said they had unprotected sex because they were drunk.
Women who were diagnosed with a sexually transmitted infection drank 40 per cent more than those who did not, showing a much stronger link between risky behaviour and alcohol consumption than previous thought.
The researchers, based in Southampton and Portsmouth, said the Government must tackle the issue of cheap alcohol and called for condoms to be provided for free in pubs, clubs and taxis.
Abortion clinics are already bracing themselves for a post-Christmas boom in unwanted pregnancies after one charity reported a record month in January this year.
The family planning service Marie Stopes International performed almost 6,000 abortions in January - a rise of 13% on the previous year.
The first detailed UK study carried out in sexual behaviour and alcohol questioned 520 people who attended one genito-urinary clinic in a city in the south of England.
A third of women in study (92 women), who attended the clinic reported a pregnancy and 41 of them had undergone a termination. Half said of those who were pregnant said it was unwanted and more than a quarter of those said they had been drinking before having unprotected sex.
The paper published in the International Journal of STD and AIDS said: "The UK has a specific problem with binge-drinking that is not seen elsewhere in Europe, and it seems highly likely that this binge-drinking culture is a risk factor for all forms of sexual risk, including sexually transmitted infections (STIs)."
Linda Tucker, one of the main authors of the study and a consultant nurse in sexual health and HIV, said: "The link between sexual risk and drinking too much is not the most original idea in he world but we now have clear scientific evidence of the relation ship. The Government needs to reflect this link both in their sexual health and alcohol strategy - which at present seems not to link alcohol and sexual risk behaviour.
advertisement
"Politicians need to tackle the issue of cheap booze and to have properly funded early intervention and treatment programmes in place."
They also found that women who binge-drink have more sexual partners than those who don't.
For men the results were not as clear-cut but the more they had drunk the less likely they were to use a condom.
The authors argue that, as the UK moves inevitably towards a 24 hour drinking culture, it is vital that the infrastructure needed to keep these drinkers safe keeps pace and is adequately funded.
A spokesman for Alcohol Concern said: "These new, and much higher figures suggest that risky sexual behaviour and binge drinking are far more bound up with one another than previously thought.
"We need also to ensure that staff working in sexual health clinics are trained to identify problem drinkers and know where to refer them for specialist advice, if they want help to bring their consumption down to safer levels".
source: The Telegraph
Monday, December 17, 2007
New DUI weapon unveiled

BELLEFONTE — Centre County's first DUI court could be up and running in the first quarter of 2008 as a pilot program designed not only to punish offenders but to treat the underlying addiction that led to their arrests, Centre County Judge Bradley P. Lunsford said.
Armed with studies and firsthand experience that show “warehousing” repeat DUI offenders in prison doesn’t work, planning is almost completed for the pilot program that will target third-time DUI offenders who have the highest tier of blood-alcohol contents — at least a .16 percent.
The announcement of the DUI court comes as the State College Police Department gets close, for the second consecutive year, to setting a dubious record.
Borough police have arrested 460 people for DUI as of Friday and are on pace to easily beat the record 484 DUI arrests in 2006, said State College police Lt. Dana Leonard.
At the same point in 2006, officers had made 436 DUI arrests, he said.
It’s an even worse picture countywide, according to statistics compiled by the office of Centre County District Attorney Michael Madeira. Last year, Madeira’s office prosecuted a record 850 DUIs.
While police attack DUI on the streets of Centre County, Lunsford, Madeira and a team of others in the justice system say the county’s first DUI court will fight the potentially deadly crime in a new way — with both punishment and rehabilitation.
“We welcome any innovative strategies, and this DUI court would be one of them, which would address these underlying issues, which would be addiction to alcohol or any other substance,” Leonard said.
The effort led by Lunsford would create a court that would not simply jail then release offenders but provide them “with the tools to maintain sobriety through judicial intervention, intensive supervision and substance abuse treatment,” according to the effort’s mission statement.
Rather than spend a mandatory year in jail, third-time offenders would do 90 days in jail and then undergo in-home detention and intensive monitoring along with counseling aimed at ending their substance abuse and addiction.
But this program will be much more difficult for offenders than serving a year at the correctional facility, Lunsford said.
“This is a much different program than going to jail and getting work release,” Lunsford said. “It’d be far easier to do the jail time. This is a very vigorous program, with intense therapeutic intervention and intense supervision.”
The pilot effort will operate early next year if federal, state and local funding comes through as county officials expect, Lunsford said.
The annual cost of the DUI court is estimated at $275,000, which would include hiring an additional probation officer for the program and cover counseling and therapeutic costs. Federal and state grants are available — both governmental levels advocate such courts — and costs also will be offset by fees imposed upon participants, the judge said.
The current practice of jailing third-time DUI offenders for a year doesn’t seem to be working, experts said.
“Essentially what we’re doing is warehousing these people in the Centre County Correctional Facility for a cost of about $60 per day,” Lunsford said. “And we’re not doing anything to address the underlying problem. This will really be one of the first attempts by a justice system to address the underlying problem, rather than just punish for the offense.”
The judge cites studies that show recidivism rates for third-time DUI offenders is about 85 percent. By comparison, the likelihood of repeat offenses by people who have gone through a DUI court is about 15 to 25 percent.
Madeira said the court likely will handle about 30 of 1,000 DUI offenses. His office does not keep statistics on how many third-time offenders are dealt with in a year, he said, but added DUIs overall make up at least a third of his case-load.
“They’ll have to do a whole lot more than sit in a jail cell,” Madeira said. “They’ll have to make changes.”
Plans still being finalized call for the DUI court offenders to spend 90 days in jail, followed by nine months of in-home detention. During that time, the offenders not only will have to wear ankle bracelets to monitor their movements but will be required to take in-home breathalyzer tests at specific times. The results of the tests, along with a photo taken of the offender as he or she takes the test, will be instantly transmitted back to a monitoring center, said Tom Young, chief probation officer for Centre County.
After the period of home detention ends, the offender will be required to wear an alcohol-detecting ankle bracelet, which monitors for alcohol use around the clock, Young said. There also will be requirements for counseling, treatment and frequent random drug and alcohol tests, all tracked by the court.
While this may be a therapeutic court with reduced jail time, Lunsford and Madeira stressed it will be far more difficult for offenders to go through, as it will force them to face and overcome their addiction.
“I’m not in this for a feel-good social response,” Madeira said. “I want to identify those who could harm someone because they have a problem. If it prevents another criminal case, another death ... that’s a step in the right direction.”
Young said the DUI court should prove a success, so long as it is staffed accordingly. His office, as it currently is staffed, could not handle a DUI court.
“It needs to be properly staffed because it is an intensive program,” Young said.
It’s also, he said, a program with great potential. There is a reason the court will start with three-time DUI offenders, he said.
“We want to start slow so we can do it right,” Young said. “Then we’re going to work back toward the second-time offenders. We can go wherever we want with this as far as expanding it.”
Centre County Chief Public Defender David Crowley also provided input for the creation of the DUI court.
“It’s at least worth a look, a pilot program, and see where we are a year from now,” Crowley said.
Pete Bosak can be reached at 235-3928.
source: centredaily.com
Sunday, December 16, 2007
Hope for the Holidays

Holidays rough but there is hope
As if the calendar wasn’t enough, the phone calls and e-mails are telling me that the holidays are upon us.
Maybe it’s the approach of a new year and the desire to wipe the slate clean, to start over and make a resolution to do better in the next year. Maybe it’s the desperate attempt to clean up in time for Christmas, to give the family something more than busted promises and disappointment.
Whatever the case may be, addicts and alcoholics often find themselves in dire straits during the holiday season.
I remember well a few of my own — trying heroin for the first time on Christmas Eve, sitting in an acquaintance’s apartment with a couple of using buddies and a drug dealer who eyed us all with a mixture of greed and contempt, never in my life having felt more alone and desperate and certain that I was about to cross a line from which there was no coming back.
Shopping for presents, paltry and meaningless, and angry with the loved ones for whom I was buying them because I would rather be spending the money on Oxycontin, and then hating myself for feeling that way.
Getting up on Christmas morning, not from the excitement of holiday magic or the desire to fellowship with family, but to sneak into the bathroom before anyone else awoke so I could shoot up and make it through the day without feeling sick from withdrawal.
Truth be told, every day is a rough one when you’re in the grips of addiction and/or alcoholism. But the pressure of the holidays and all of the expectations on us — to be social, to be kind, to care about others more than we care about ourselves — goes against the self-centered nature it takes to survive as an addict.
We’re anti-social, we don’t like spending our money on anything but what can get us high and we despise who we are and what we’ve become — being around other people, buying them gifts, taking stock of ourselves like most people do as a new year dawns; all of those things make us more aware than ever of the train wreck that our lives have become.
For some, such increased awareness leads to more feelings of hopelessness and desperation. That’s why suicides among addicts increase during the holidays; sometimes, death seems a preferable alternative to facing the disappointment in the faces of those we’ve let down. Others go all out for the last few weeks of December, resolving to stop using and turn our lives around come Jan. 1.
Still, others want to put the brakes on immediately and discover just how difficult it can be getting into treatment in time for a clean and sober Christmas.
There is hope for the holidays, however.
There’s no magic pill, no instant cure-all, that will make addiction and all of its problems go away. Addicts trying to get clean need to realize that they didn’t become addicted overnight and didn’t wreck their lives overnight; therefore, they’re not going to clean up and straighten out all of their problems overnight, either.
Recovery takes time, and it’s a rocky road at first. It takes willingness and commitment and acceptance, and sometimes those with a drug problem have more of one than another or a little of all three but not what it takes to stop getting high.
The hardest step is that first one — the one where we look in the mirror and realize we can’t go on like we have been. Once we take that step and resolve to do anything it takes to get better, the next get a little easier.
Whether it’s calling around to treatment centers or finding a 12-Step meeting or calling a minister or getting into therapy, there are baby steps those in active addiction can take to putting their lives back on track and salvaging what remains of this holiday season. Like I said, it won’t make everything go away. There won’t be any Christmas miracles that get us out of debt or repair the emotional and spiritual damage we’ve done to our family members. There won’t be an overnight cure where we wake up on Christmas morning and find ourselves rid of the obsession and compulsion to get high.
But there will be hope. I’m living proof, and so are hundreds of others in recovery like me, that addiction can be arrested and that a new way of life can be found. It’s never too late and it’s never too early to stop looking for it, whether it’s Dec. 25 or June 25. The holidays don’t have to be bleak, and they don’t have to be meaningless.
Any addict can lose the desire to use and find a new way of life, if they’re willing to put as much effort into staying clean as they were into getting high.
That’s the promise of recovery, and that’s the message I hope those affected by addiction — the addicts and the families and the friends and the loved ones — get from these words.
Steve Wildsmith is a recovering addict and the Weekend editor for The Daily Times.
Thursday, December 13, 2007
Holiday Blues Trigger Increased Alcohol, Drug Use

Better Tomorrow has seen a 50 percent increase in requests for drug and alcohol interventions across the country since October, a spike clinic therapists attribute to the holiday blues.
"Families are usually the biggest stressors around the holidays because mental health problems often have their roots in difficult family relationships," said Dan Chapman, director of A Positive Outcome Intervention Services at A Better Tomorrow in Murrieta. "People use more alcohol and drugs as a coping mechanism, and that sets the stage for a crisis. We see this happen every year as we approach the holidays. It's a good thing people are calling, of course, because this means more people who need help are getting into treatment."
Addicts usually deny that they have a problem, even when their addictions are tearing apart their families or leading them down a path toward unemployment or financial ruin. Addicts typically will not listen to advice from their families, either. That's why a professional interventionist is often needed to convince the addict to seek professional counseling and treatment.
A Better Tomorrow provides professional intervention services as well as residential and outpatient treatment programs for alcohol abuse as well as addiction to illegal and prescription drugs.
"People often try to minimize the significance of marijuana addiction as if it's less damaging than cocaine or methamphetamines," Chapman said. "But marijuana addiction still leads to employment problems, alienation from family members and other mental health problems."
Addiction to prescription painkillers is also becoming an increasing problem, Chapman said, citing A Better Tomorrow's clinical experience as well as a recent statistics compiled by the Substance Abuse and Mental Health Services Administration (SAMHSA), which found that nonmedical use of prescription drugs among young adults had increased from 5.4 percent in 2002 to 6.4 percent in 2006.
source: emaxhealth.com
Tuesday, December 11, 2007
Online Recovery Meetings
There are many different ways that members of support groups can gather together online from email discussion groups, real-time chat rooms, message boards and now voice chat.
With the phenomenal growth of the Internet in the past few years, as millions of new users logged on for the first time, many of them were members of various recovery groups. Naturally they began to find ways of gathering together for mutual support.
The following is a description of some of the ways online "meetings" are conducted, how they work, and how to find them.
Email Groups
One of the most popular methods of holding topic discussion over the Internet are email discussion groups. The main advantage to email groups is that the meetings are conducted 24 hours a day seven days a week, but members can join in the meeting at any time that is convenient for them.
Typically, members of the group send messages to a single email address which is then forwarded to all members of the list.
Usually someone "leads" the meeting by introducing a topic and then other members share their experience, strength and hope on that topic.
When members are "ready" for a meeting, all they have to do is check their email and "shares" on the topic are downloaded into their in-boxes, which can be read at any time. If members wish to share on the topic, they can just click on the Reply button and add their comments.
Real-Time Chat Meetings
Many people prefer attending real-time chat meetings online because they "feel" more like face-to-face meetings. The meetings take place in "real time" meaning that as soon as participants type a line on their screen and hit the Enter key or the Send button, their message is seen immediately by everyone else in the chat room.
Chat meetings are also like face-to-face meetings in that a lead or chairperson introduces a topic and others in the room take turns sharing on the topic. At some meetings, the chairperson will also "read" the opening and closing statements, just like at a face-to-face meeting, by copy-pasting the text files.
Unlike email meetings however, participants do have to be at a certain web site and a certain time to join the meeting, but those participants may be joining the meeting from locales across the globe.
Message Boards
Message boards or bulletin boards are one of the oldest methods by which members of the recovery community first began to gather together on the Internet. Like email meetings, participants can join in any time, even weeks or months after the topic was first introduced.
Although message boards or "forums" are probably less like face-to-face meetings than any other methods discussed here, they do have the advantage of carrying the message long after messages are first posted. Anyone can begin a discussion by starting a "thread" on the board to which others can reply.
A thread begun today in which participants discuss a particular topic or situation they are dealing with now, can help and support others who visit the board months or even years from now. Although the are becoming less popular than they once were, there are still many still active. Here are two examples:
oice Chat and Video Chat
The advent of new technology has now brought about "voice chat" meetings in which participants can actually hear each other share on the meeting topics. In the "virtual" world of the Internet, these meetings may be the closest to the "real thing" that we have available thus far.
With the use of a microphone and speakers, participants can talk and listen to others in the room, who may be from all over the world. Even those who do not have microphones can share by typing their messages to the screen.
Although "voice chat" meetings are relative a new addition to online recovery, they have become very popular.
Technology has also brought about the ability to hold video chat meetings, which allow participants to see others in the meeting via Web cameras, or cams.
Source: http://alcoholism.about.com
Monday, December 10, 2007
Warning Signs of Alcoholism

You regularly use alcohol as a way of coping with feelings of anger, frustration, anxiety or depression.
You regularly use alcohol to feel confident.
You get hangovers regularly.
Your drinking affects your relationships with other people.
Your drinking makes you feel disgusted, angry or suicidal.
Other people tell you that when you drink you become gloomy, embittered or aggressive.
You need to drink more and more to feel good.
You stop doing other things to spend more time drinking.
You start to feel shaky and anxious the morning after drinking the night before.
You drink to stop these feelings.
You start drinking earlier in the day.
IF YOU NEED HELP NOW PLEASE JOIN US AT The Sober Village where you do not need to be sober to join, just the desire to some day do so!
Saturday, December 8, 2007
Group wants to turn old church into 12-step recovery center

Amidst serious opposition from some of the neighbors, the Oshkosh Common Council on Tuesday will consider the possibility of turning an old church into a place for 12-step recovery meetings.
Kornerstone Recovery Inc. wants to move from its current location on Oregon Street and set up an all-day 12-step recovery center on the corner of Evans Street and E. Parkway Avenue in an old church.
The building is surrounded by a residential neighborhood and would need to be classified as a community center in order for the recovery group to hold meetings there.
The Oshkosh Plan Commission did not approve a conditional use permit for the center during its meeting last week, mostly because of concerns from the neighbors. However, the commission is only authorized to recommend action, and the issue will still go in front of the council for a vote.
Ken Reuhl, president of Kornerstone Recovery, said the facility would be open between 9 a.m. and 8 p.m., and about 80 percent of the 12-step meetings would be closed to non-addicts.
He said he was frustrated that the plan commission did not recommend approving a conditional use permit.
"We are a property of hope and healing, which that property there has stood for, for many years," he said. "Hope for that area of the community."
The 12-step meetings would be limited to Alcoholics Anonymous, Narcotics Anonymous, Alateen and Al-Anon, all of which the group does at its current location on Oregon Street, Reuhl said.
Evans Street resident Victor Mitchell lives a couple of houses away from the property where the new facility would be located. He said he is against having it there.
"It should stay in more of a business oriented neighborhood," he said. "I mean, for goodness sakes we need them, but there should be more of a buffer."
Reuhl said concerns about dangerous people in the area are unfounded.
"There's professional people, attorneys, doctors, successful business people that are in recovery," he said.
Sharron Taylor, who lives on the 900 Block of East Parkway Avenue, said she's not against 12-step programs, but having an all-day facility down the street from her house could pose practical problems.
"I'm not opposed to people getting help and going to meetings and that kind of stuff because I think just because they've had problems in the past doesn't mean that they're always going to be bad necessarily," she said. "But if they're going to be standing around and parking in front of my house all day, then yes, I have a problem with that."
source: Oshkosk Northwestern
Crystal Lindell: ![]()

![]()
![]()

![]()
![]()
![]()
![]()
![]()
![]()
![]() (920) 426-6668
(920) 426-6668![]() or clindell@thenorthwestern.com.
or clindell@thenorthwestern.com.
Friday, December 7, 2007
Drinking in the U.S. Remains Unchanged

About 1/5 Are Binge Drinkers
The latest government statistics show a decrease in the use of illicit drugs over the past four years, but the number of people who consume alcohol remains essentially the same, with more than half of everyone over the age of 12 reported as drinkers.
Each year the Substance Abuse and Mental Health Services Administration sponsors the National Survey on Drug Use and Health (NSDUH), in which 67,500 persons are interviewed. The NSDUH is the government's primary source of information about the use of illicit drugs, alcohol and tobacco in the general population of the United States.
The 2006 survey indicated very little change in drinking habits, with about half of the population (50.9 percent) reported as alcohol drinkers, about one-fifth binge drinkers and about seven percent listed as heavy drinkers.
Binge Drinkers and Heavy Drinkers
Binge drinking is considered having five or more drinks one occasion at least once in the past 30 days.
According to the survey results, 23 percent, or about 57 million people over age 12, met that definition.
Heavy drinking is considered binge drinking five or more times a month. The 2006 NSDUH survey indicated that an estimated 6.9 percent of the population, about 17 million people over age 12, were heavy drinkers.
Drinking Rates Higher for Young Adults
For young abuts, between the ages of 18 and 25, the rate of binge drinking and heavy drinking is almost double that of the general population. In 2006, the rate of binge drinking in this group was 42.2 percent and the rate of heavy drinking was 15.6 percent.
The survey also showed that the rate of binge drinking in adolescent drinkers -- those ages 12 to 17 -- is about 10.3 percent, with the percentage of heavy drinkers at 2.4 percent. All of these rates are basically unchanged from the 2005 NSDUH results.
Drinking Rates by Racial Groups
For underaged drinkers, those age 12 to 20, the survey indicated past month alcohol use among these groups as:
* 18.6 percent among blacks.
* 19.7 percent among Asians.
* 25.3 percent among Hispanics.
* 27.5 percent among those reporting two races.
* 31.2 percent among American Indians or Alaska Natives.
* 32.3 percent among whites.
Of the above groups, the only significant change since 2005 was with American Indians or Alaska Natives, who reported only a 21.7 percentage of drinkers in 2005.
Pregnant Women Drinking Less
Here are other findings of the 2006 NSDUH:
* Binge drinking rates for underage drinkers have remained unchanged since 2002, with about 28.3 percent of those aged 12 to 20 reported as drinkers and 19 percent binge drinkers. About 6.2 percent were heavy drinkers.
* Binge drinking during the first trimester of pregnancy dropped from 10.6 percent to 4.6 percent for women aged 15 to 44. This is the only group that saw a decrease in drinking rates.
* An estimated 12.4 percent of persons aged 12 or older reported driving under the influence in the past 12 months. That percentage corresponds to about 30.5 million people.
Sources:
Substance Abuse and Mental Health Services Administration. "Results from the 2006 National Survey on Drug Use and Health: National Findings" Sept. 6, 2007.
Thursday, December 6, 2007
Abstinence best for recovering alcoholics

Complete abstinence from drinking offers alcoholics the best chance of a lasting recovery -- though it may not work as well for the youngest alcoholics, a U.S. government study suggests.
In a study that followed nearly 1,800 alcoholics over 3 years, researchers found that those who abstained from alcohol were less likely to suffer a relapse than those who had only cut their drinking to modest levels.
At greatest risk were those who were no longer suffering symptoms of alcoholism at the beginning of the study, but were still drinking fairly heavily.
Lead author Dr. Deborah Dawson of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and her co-authors also found that the chances of lasting success with abstinence varied by age. Among alcoholics younger than 25, abstainers were no more likely to stay in remission than those who were still drinking heavily at the study's start.
The findings suggest that young alcoholics need more help in achieving a lasting recovery, Dawson and colleagues report in the journal Alcoholism: Clinical and Experimental Research.
The study included a nationally representative sample of U.S. adults who, at the outset, were in remission from alcohol dependence. Just over 38 percent had completely stopped drinking. A similar percentage were considered "low-risk" drinkers; they were free of alcoholic symptoms - such as craving and physical withdrawal symptoms when they weren't drinking -- but were drinking at moderate levels.
The rest were free of alcoholic symptoms but were still drinking at levels believed to put them at high risk of relapse -- 14 or more drinks per week for men, or 7 or more for women.
Three years later, 1,772 study participants were interviewed again. Half of the high-risk drinkers had an occurrence of some alcohol abuse symptoms, while 10 percent had relapsed into full-blown alcohol dependence. The corresponding figures for the abstainers were just 7 percent and 3 percent.
Among low-risk drinkers, 27 percent reported some symptoms of alcohol abuse, while 4 percent had relapsed.
When the researchers looked at the group by age, however, they found that alcoholics younger than 25 had the most difficult time with long-term recovery -- even if their chosen route was abstinence.
Nearly 30 percent of young abstainers were suffering alcohol abuse symptoms 3 years later, and almost 12 percent had relapsed into dependence.
"The first thing we can take from these findings is that we need to learn a lot more about the best treatment approaches for younger patients," said Dr. Mark L. Willenbring, director of treatment and recovery research at the NIAAA.
Most alcoholism treatment studies have been in middle-aged adults, he told Reuters Health, because the youngest alcoholics are typically not the ones who seek treatment.
According to Willenbring, who was not involved in the study, researchers need to find ways to reach out to younger alcoholics where they are -- on college campuses, for example, or in emergency rooms after a binge.
One key obstacle to successful treatment, Willenbring noted, may be the context in which young alcoholics drink. Whether they are in college or not, young adults' social life often centers on bars and drinking, he pointed out. Younger patients may need more help in dealing with these social influences.
SOURCE: Alcoholism: Clinical and Experimental Research, December 2007.Wednesday, December 5, 2007
Cross Addiction
An addict I knew had a bad relapse. We couldn't figure out why. A reason may have been his use (not abuse) of an over the counter flu medication. It contained codeine, which is obtained from opium or prepared from morphine. He was a recovering heroin addict and the codeine sparked cravings. His flu nearly cost him his life.
The many pills and potions I was prescribed in hospital to treat my depression and anxiety, I became addicted to. To this day, I still crave Valium and Chloryl Hydrate on occasions - just out of the blue. But luckily those feelings are just flashes now, but they still serve as a warning.
Many alcoholics/addicts who go into recovery, never actually do. They simply swap one drug of dependence for another. An example would be someone who gives up alcohol and then is using valium long term for their "nerves". The "nerves" are actually protracted withdrawals, their bodies are never given a chance to actually start recovering. This is called cross-addiction. These drugs are usually prescribed to addicts in the first twelve months of recovery. Way too soon in most cases. The brain doesn't seem to differentiate between drugs.
I am a heavy tobacco smoker. I tried giving it up a couple of years ago by chewing nicorettes. Now I smoke and chew nicorettes. My caffeine consumption amazes people. There has been months where I consumed no other fluids apart from caffeinated drinks. So I guess if it really boils down to it, you could consider me not "recovered". But I am happy where I am at, and tobacco and caffeine does not seem to spark cravings for other drugs. It seems to be the exception to the rule. What are your views on this?... I'd be interested to know. Maybe I'll give up some day, maybe I won't, it's not an issue for me at the moment. Cigarettes and coffee have never caused me do the things I did whilst under the influence of other drugs and they definitely do not make my life unmanageable.
This may anger the non-smokers out there, but giving up tobacco and coffee early in recovery after giving up alcohol and/or other drugs can be quite dangerous. The body can go into overload, and you can end up right back where you started. And no, I'm not rationalizing, I'm serious.
I've got a feeling I may get a lot of email on this subject................
I take no other drugs. I am very careful not to. No liqueur chocolates, no medications containing codeine. I was very scared when I had to have a general anesthetic that I would wake up with withdrawals, or worse still, wake up during the operation because of my tolerance to that class of drugs. I discussed it with my doctor, who I was lucky to have - he understood addiction and he bumped up the levels of anesthetic. I regained consciousness fairly quickly, but at least not while I had the scalpel in me! And yes, I did suffer from mild withdrawals....
These are the things that an addict needs to keep in mind going through day to day life. A great many things that others take for granted, we can't have - or they have higher risks associated with them. It's as simple as that. Remember to carefully read the labels of any medication you are taking and find a doctor who understands your circumstances and the disease of addiction. At this point, I would like to state that I have no professional medical qualifications and I do not wish to turn anyone from their doctor prescribed treatments. I am only suggesting that you be aware of the dangers of cross-addiction by questioning any prescription or treatment you are given.
If you are not sure about the medication you are currently taking, a good source of information is http://www.rxlist.com/ . It has a huge listing of medications and associated issues. If your medications have a warning label on them that says "may cause drowsiness", you can bet that it contains some sort of MAS (Mood Altering Substance). Sometimes these medications will be necessary, but please, handle with care.
We are on the road to recovery and numerous emotions boil over in us. They can be quite overwhelming, we aren't used to dealing with them "straight". The most prevalent ones are depression and anxiety. Some doctors approach these conditions with the prescription of anti-depressants and tranquilizers. Does that seem right to you?
Doctors abide by what is known as the Hippocratic Oath. The oath had its origins from Hippocrates who is considered to be the Father of modern medicine. He also stated "It is more important to know what sort of person has a disease than to know what sort of disease a person has." This has special bearing in the case of anxiety and depression in the recovering addict. If your doctor is unaware that you have a substance abuse issue, he/she may prescribe totally unsuitable medications that could ultimately bring about your undoing. I came across a scenario like this only a few weeks ago. A close friend of mine who previously had cocaine problems was prescribed a tranquilizer - it had some undesirable effects.
Once again, these medications have their place, but not so much in recovery. The emotions you will experience are normal, they will pass. Anti-depressants and tranquilizers may act as a thin bandage over a gaping wound and may worsen the damage already done. Part of recovery is about dealing with emotions and problems without the use of drugs or "medicines". Medication does play an important part in the initial withdrawal stages, as detoxing can be potentially fatal. If you are currently taking anti-depressants and/or tranquilizers and decide you want to try to get along without them, ensure you discuss it with a qualified health professional first. Sudden cessation of the medication can be dangerous, and there are cases where they are necessary.
Well, my ash-tray is overflowing and my coffee cup is empty....I better go get another!
Michael Bloch
michael@worldwideaddiction.com
http://www.worldwideaddiction.com
Tuesday, December 4, 2007
Heroin addiction

Heroin addiction is a very serious addiction that has a high rate of mortality. There are many severe health concerns that coincide with heroin addiction, including the worst, fatal overdose, as well as collapsed veins, from injecting heroin, AIDS disease, from unprotected sex and sharing needles with many other people who have heroin addictions, and hepatitis, from needles and unprotected sex as well. A person who has a heroin addiction, when asked about the feelings that heroin gives them, usually will say that the immediate feelings of the drug give a sense of euphoria, causes a feeling of heaviness in the limbs, dry mouth, and sporadic exchanges of felling sleepy, and then feeling alert. Heroin acts as a depressant on the central nervous system, which then causes the body to experience lowered mental capabilities.
When a person who has had a heroin addiction for an extended period of time continues to use, there are detrimental long-term effects will begin to set in. These long-term effects associated with heroin addiction can include, collapsed veins, cellulites, which are bacterial skin infections, an infection in the heart lining and valves, liver disease, and abscesses, which are pockets filled with pus inside infected tissue. Pneumonia is also a complication linked to heroin addiction that can occur due to bad health resulting from a weakened immune system, or continued depression on the person with a heroin addiction’s respiratory system.
The drug heroin is considered to be not only a psychologically addictive drug but a physically addictive substance as well. When a person who has a heroin addiction stops using heroin, either by choice or force, they will immediately begin to feel the onset of painful withdrawal symptoms that usually include anything from nausea and depression to convulsions, increased heat rate, and even heart attacks. While the person who has a heroin addiction usually uses heroin to feel good and to lift up their spirit and feelings toward life and others in order to get them through the day, continuing this detrimental behavior will, without a doubt, lead to an increased tolerance of the drug, and a heightened heroin addiction. This higher tolerance for heroin makes the heroin addiction and the dependence on the heroin even more dangerous for the user, as its effects become more prominent, and the warning signs will often begin to appear more noticeable to family, friends, and other close ones around them. There are some important warning signs of heroin addiction to look for that anyone should know who knows someone suspected of having a heroin addiction. Some of those signs include, but are not limited to:
-
falling asleep at abnormal times, sometimes mid-conversation
-
wearing long shirts or pants at inappropriate times to cover up track marks left by injection
-
syringes used for injection
-
burnt spoons used to melt the powder into injection form
-
razor blades, rolled up dollars or other tubes used to snort heroin
-
baggies with a powder residue,
-
unused balloons tied off, which are used to transport the heroin
-
tourniquets used to tie off blood flow to inject the heroin
Even though there are so many different drug treatment centers and programs offered all over the world for heroin addictions, even if they successfully succeed at completing the rehab program, there is still always that very real possibility for relapse for anyone who has ever been addicted to any drug, particularly those who have ever had a heroin addiction. Relapse prevention programs were created as a part of the rehabilitation therapy at many drug rehab centers, and some of the relapse prevention programs even extend longer, even after the patient has left the drug treatment facility. These programs were created to give those with heroin addictions and other drug and alcohol addictions more tools and ammunitions to prepare themselves for the temptation to use again, and the ability to successfully fight it once they return to their lives on their own.
Through studies and experiments, experts have recognized a pattern of certain life situations and psychosocial factors that they have determined can be linked to increasing the likelihood or risk of a relapse of someone with a heroin addiction. Some of these factors include:
-
Mental stress or anguish – Many doctors believe that stress is the leading predictor of heroin addiction, as well as other drug addiction relapse. It’s been identified that in opiate addicts, those with high stress levels were strongly predictive to continue to use drugs. There have also been studies done on animals that have confirmed the idea that heightened stress, anxiety, or pressure can lead to a relapse of the behaviors of the previous heroin addiction, or other drug addiction.
-
Negative emotional states, such as depression
-
Interpersonal problems
-
A lack of support from family or friends, or simply a lack of family or friends
-
Underdeveloped coping skills or problem solving abilities
-
Loss of the desire to stay sober, or giving up
There is really no clear cut way to determine how likely it is for someone with a heroin addiction to relapse, or someone with another type of addiction. What is known is that any one of the above factors listed, or a combination of them, have the potential to cause, or lead to the start of a relapse. It’s important that if you know anyone with a heroin addiction or any type of addiction that you remember that they need your support.
Let them know that you are always there for them and that you care whether or not they beat the heroin addiction and choose to stay sober. Knowing that they’re not alone can really make a difference, because a drug rehab center alone may not be enough.
Monday, December 3, 2007
Alcohol program review
A change in leadership at the Alcohol Abuse Deterrent Program presents an opportune time to review the entire program – not only its management, but its effectiveness, safety and value in light of new developments in alcohol-abuse treatment.
The non-profit program’s board of directors recently sent a letter to Terry Yeiter, executive director of AADP since 2000, asking him to step down. Win Rood, the board’s chairman, said the board had lost confidence in Yeiter’s management abilities, including the lack of a sound accounting system for medication distributed by the program.
The rumor mill suggested there was medication unaccounted for and reports of overcharging. Rood said an investigation found AADP actually had more pills than records showed, but they were at a different treatment location.
AADP was established to provide an aversion-therapy alternative to incarceration for repeat drunken-driving offenders. Court-ordered participants take Antabuse, the brand name for disulfiram, which blocks the body’s ability to process alcohol and causes discomfort or illness when taken in combination with alcohol. Last year, AADP administered Antabuse or breath tests to about 1,500 people a week. Offenders are required to pay for treatment.
Questions about the program’s cost have long circulated. According to figures from the 990 form filed with the Internal Revenue Service, Yeiter earned $73,170 in 2006. That amount was down from 2005, when he earned $85,239 in salary and benefits and 2004, when he earned $91,897. Five other AADP employees earned more than $57,000 in 2006, and contracts for medical and legal services totaled more than $319,000.
To its credit, Rood said the board will re-evaluate the organization’s structure. A full audit will be performed.
In its inquiry, the non-profit board should engage in serious self-examination beyond any search for wrongdoing or mismanagement. Certainly, AADP is a less-costly alternative to locking up repeat DWI offenders, but is it the most cost-effective alternative? Do the medical and constitutional questions about Antabuse treatment warrant its continued use? The program has been the subject of legal challenges, and there are questions about the drug’s effect on the liver.
Allen Circuit Judge Thomas J. Felts, who orders some offenders to the program, said that he is re-evaluating the best course for felony drunken-driving cases in light of the developments at AADP but said the program has been doing a good job in spite of the director’s departure.
“We are in good communication about what steps they are taking,” Felts said. “What direction we take will be based in large part on what their audit and investigation finds. It will help me in my determination of where the board should go.”
The judge said the prosecutor’s office and adult probation will also help to determine the outcome. “We’re all partners in this,” he said. “It’s a countywide approach.”
The judge said that none of the options for handling felony cases is perfect, but the goal would be to find the best.
Some state and local corrections systems are turning to the use of technology, including a new ankle-monitoring system that detects alcohol consumption by the wearer. The device is in use in 44 states, including Indiana. Felts said he was at a conference where Indiana University medical school representatives reported high error rates with the system, but he acknowledged that some judges and probation officials in Marion County were pleased with results there.
AADP has served the probation and court system in Allen County for almost two decades, undoubtedly saving lives in the process. But every organization demands review over time. The problems that arose in the deterrence program and resulted in its director’s departure prove the review at AADP is overdue.
source: Journal Gazette Forth Wayne, Indiana
Sunday, December 2, 2007
I know from experience: Drug treatment does work

As a person in recovery from addiction, I can speak to the devastation addiction brings. By the time I was in junior high, I was using drugs daily. This continued until I was in my mid-30s. By then I had given up custody of one of my two children. I had given up a promising career and given up hope of being in a healthy relationship. I had nearly given up on life several times.
By 1994 I was addicted to heroin. I remember feeling that my addiction was not out of control because I had a roof over my head and I had retained custody of my other child. I was not willing to see that I was in an abusive relationship and nearly destitute. I made good money working construction but ate from the food bank for almost half the year. I reached out for help in late 1994. When I called to get into treatment, I was given an assessment and told that the waiting list was about six weeks long. I began treatment just before Christmas that year. I was fortunate.
Today in Alaska, there are fewer treatment programs, fewer available beds or treatment slots. It is not uncommon for addicts to reach out for help only to be told that the waiting list can be three to six months. Detoxification programs are nearly nonexistent. They are only a part of a continuum of care that needs to provide appropriate levels of care for treatment to be successful. After 15 years of flat funding or decreases, our programs are barely able to meet the increased need for services. Nearly 54,000 Alaskans, or 11.2 percent of the population of the state, was addicted to alcohol or other drugs according to a recent study (McDowell Group, 2005).
The fallout from these addictions can be seen in our courts, jails, hospitals and foster care system. Families are torn by violence, death and disease associated with addiction to alcohol and other drugs. There are effective solutions to these problems and our state needs to take an honest look at where we are and where we are going if we don't support the programs that can provide those solutions.
Due to the stigma attached to the recovery and treatment community, society at large does not hear the success stories. I am here to testify that treatment saved my life. It provided me with the ability to stop using long enough to take an honest look at my life and learn the skills needed to live and enjoy my life without drugs, including alcohol. Treatment programs have helped thousands in our state go on to live as productive members of their communities. In order for this to be available, our state and local communities need to support treatment programs and recognize them as assets rather than liabilities.
Money to fund treatment programs is a wise investment. Even though some people relapse, it should not be used as a measure of success or failure of a program. People can return to communities as productive persons. Families can be reunited. Court systems and prisons can be relieved of some of the burden as people cease criminal behavior. For me, after treatment I was able to return to work, learn a new trade, rebuild my family and become active in the recovery community. I went from being nearly unemployable to holding down two positions as well as being a full-time college student. Because of the help I received in treatment, I found support in my community to continue my recovery. I no longer need to self-medicate to navigate my life. Now, I am physically and emotionally available and an asset to my family and community. A treatment program saved my life, just as treatment has for many Alaskans. We need to ensure that programs are available when people reach out for help.
By ANNA SAPPAH
Published: December 2, 2007Anna Sappah serves on the Governor's Advisory Board on Alcohol and Drug Abuse. She is executive director of the Substance Abuse Directors Association of Alaska Inc. and a tobacco policy specialist for Akeela Inc.
source: Anchorage Daily News
Saturday, December 1, 2007
Cylce of Addiction
In the midst of all this suffering, how can there be a way out? Is there any hope of defeating the monster and living a drug-free life again? A life before pills, bottles, needles, and powders? A life where you had a family who loved you, a job that you liked, and friends that weren't shoving needles in their veins? A life where there was no monster?
Yes, there is! As hopeless as it sounds, you can have your life back. No matter how tightly your addiction holds you, you are stronger. You can break that hold forever. Recovery won't be handed to you; you will have to work for it. Your addiction had a beginning; recovery also has a beginning. It starts with a choice – your choice to take back what belongs to you; your life, your health, and your spirit. Things that you thought were gone forever can be restored if you make that choice and mean it.
There is no "right" or "wrong" way to recover from addiction; there is only your way. On your journey to recovery, you will meet friends along the way who can help you when you falter, speak to you about hope when you're feeling hopeless, and lend you strength when yours is weak. When was the last time you slept through the night without drugs, enjoyed a meal, or played a game? As you recover, small things that you once took for granted will play a vital part in your life; health, nutrition, fitness, spirituality, restful sleep, affection, fun, and laughter!
Drug addiction is a cycle. You started with recreational use, believing that you can fully control your drug use. It become more frequent, and then even more frequent until your mind and your body were owned by addiction, the monster you created. However, recovery is not about self-blame. It is about personal responsibility and a total lack of denial about your addiction. Only then can the cycle of recovery begin.
Breaking the cycle of addiction
The number of Americans over age 12 using illegal drugs on a regular basis is in excess of 15 million. Each year more than 15,000 people die drug-related deaths. How could something so harmful be so popular? It’s really quite simple.
A feeling of acceptance. No pain. Complete and utter addiction. In most cases, a blatant disregard for life. Not all drug users start out with a blatant disregard for life and none start out with an addiction. Some just fall into drug or alcohol addiction by peer pressure or the temptation of having the substances close at hand in the home, perhaps.
In other cases, however, there is persistent pain. It can be emotional pain from childhood, like divorced parents and an absentee father, or emotional pain from adulthood, like the death of a loved one. It can even be physical pain from an old injury or botched surgery. The pain leads to depression and withdrawal and there seems to be no way out.
Numbing the pain seems the only option, and so begins the cycle of addiction. Soon, the body becomes more resilient to the effect of the drug or alcohol. A person resorts to higher and stronger doses, only to find themselves withdrawing further into depression and addiction. Impulse control becomes a thing of the past. Suddenly, the addiction progresses to the point where nobody and nothing matters as much as the next joint, the next drink, the next 8-ball.
Intervention may be required to isolate the person, cutting them completely off from their supply that feeds their addiction. They can then perhaps sober up enough to admit they need help. A drug rehab program is typically the next step, but only with a commitment by the student. It is an extremely difficult process of learning to love oneself again, learning to be self-sufficient and cope without fueling substance addictions. One must ultimately come to terms with the fact that the addiction is a problem and the problem has got to stop. Breaking through the denial to achieve a fierce desire for a better, healthier life is a fundamental building block of breaking the cycle of addiction.
Source:http://www.narcononstonehawk.com/addiction_cycle.php

